How dangerous is the coronavirus?
There is still much that is unknown
First and foremost, it is really important to know that as of today (February 17, 2020), there is still much we do not know about SARS-CoV-2 (i.e. the official name of the novel coronavirus) and COVID-19 (i.e. the official name of the disease caused by SARS-CoV-2). This uncertainty makes this question difficult to answer with a short or simple response.
However, epidemiologists and scientists from around the world are making rapid and significant real-time progress in understanding the nature of this novel coronavirus. Earlier today, a comprehensive report from the China CDC was released on over 70,000 individual cases in China, which included data for 99% of confirmed cases globally as of February 11th, 2020.
There is very little doubt that COVID-19 is dangerous, but just how dangerous requires a much deeper dive. Here were some of the key takeaways from this report and other research I have done on the topic.
(1) COVID-19 is highly contagious
A main finding of this characterization and exploratory analysis of the first 72,314 cases of COVID-19 found in China in the 40 days between first recognition of the outbreak of pneumonia with unknown etiology on December 31, 2019 to the end of the study period on February 11, 2020 is that this novel coronavirus is highly contagious. It has spread extremely rapidly from a single city to the entire country within only about 30 days. Moreover, it has achieved such far-reaching effects even in the face of extreme response measures including the complete shutdown and isolation of whole cities, cancellation of Chinese New Year celebrations, prohibition of attendance at school and work, massive mobilization of health and public health personnel as well as military medical units, and rapid construction of entire hospitals.
Let’s re-examine the COVID-19 timeline:
Late December 2019: A cluster of pneumonia cases of unknown origin appears in Wuhan, the city now at the epicenter of this epidemic.
December 31, 2019: Alert issued by the local Wuhan Municipal Health Commission to the China CDC and a notification was sent to the World Health Organization about this outbreak.
January 7, 2020: The pathogen was identified as a new type of coronavirus, and given the name 2019-nCoV. It was now learned that this virus was closely related but distinct to the one that caused the SARS crisis in 2003.
January 11, 2020: The first death is reported (person died two days earlier). The Wuhan Municipal Health Commission issues its first public report announcing this novel coronavirus[3] and starts issuing daily update reports.
January 20, 2020: 7 confirmed patients have now died, the virus has spread outside of Wuhan, and this becomes a national issue. China’s National Health Commission takes over primary responsibility.
January 23, 2020: China announces unprecedented quarantine operations in major cities ahead of the Lunar New Year holiday.
In the roughly 1-month period following the first inkling that this might be more than just another flu outbreak, the number of cases went from 104 to +653 to +5,417 to +26,548 roughly every 10 days. In other words, every 240 hours, the number of cases was increasing between 5 to 8 times.
This is retrospective data — after confirming cases through nucleic acid testing, individual cases were interviewed to determine (by examining symptoms or history of contact with known infected) the approximate date when they likely contracted the virus. It provides the most accurate view of how quickly this thing spread (note: this data does not provide an accurate view of total number of actual infections — confirmed cases very likely only represent a small fraction of total infections).
There is an epidemiological term called R-naught (or R0) that measures the relative contagiousness of an infection. While I have not yet seen any re-calculations based on this new and comprehensive dataset, previous calculations have placed it in the same range as SARS but lower than measles.
That is to say, it is highly contagious. But before panicking, let’s take a deeper dive into some of its other important characteristics.
(2) COVID-19 disproportionately affects older people (and those with pre-existing medical conditions)
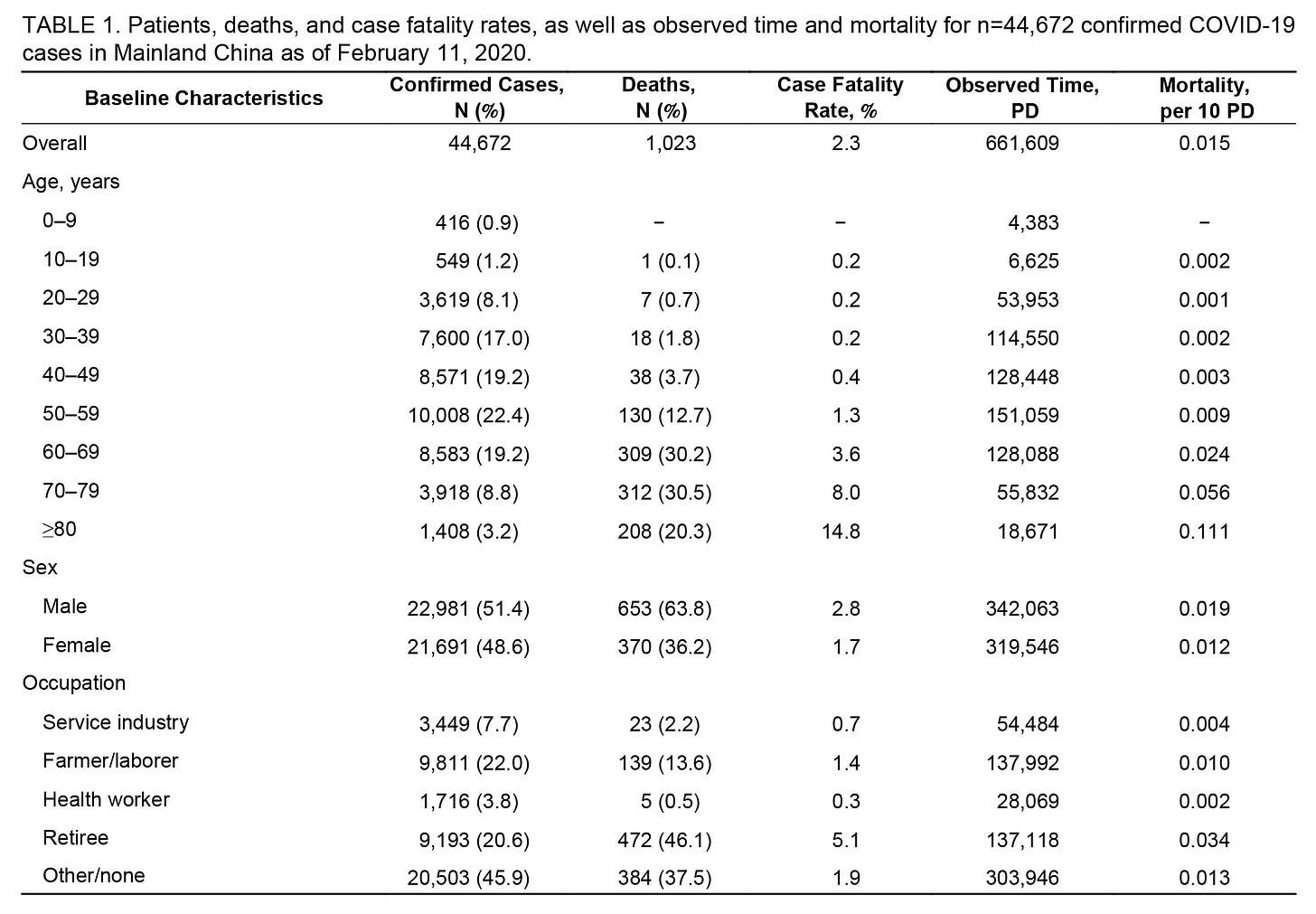
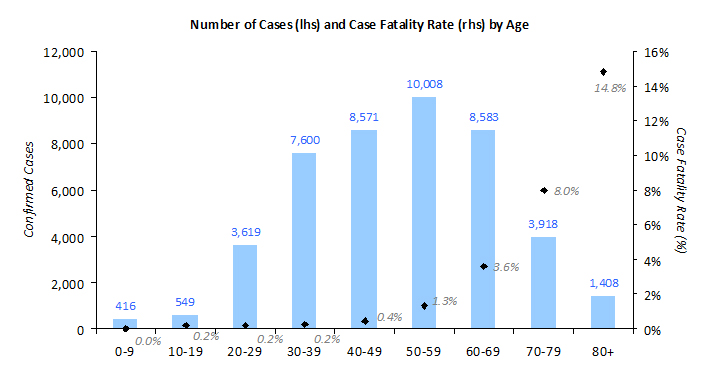
Detailed demographic data was released in the China CDC report, which confirmed analysis from earlier reports (here, here and here; based on much smaller samples) as well as reports from outside of China (Hong Kong and Singapore) that older people are disproportionately impacted by COVID-19.
First, it appears that younger people have much more resistance to SARS-CoV-2 taking hold in their bodies when they are exposed to the virus. For example, patients under the age of 20 comprised only 2% of the confirmed cases (note: some of this may be due to adverse selection bias, which I will discuss in the next takeaway).
Second, once younger people are infected with the virus, survival rates are higher. As of February 11th, there has only been a single person (out of nearly a thousand cases) under the age of 20 that is confirmed to have died from COVID-19.
Meanwhile, the case fatality rate increases exponentially with each successive decade after the age of 40. Based on these reported case fatality rates, if you are over the age of 80, you are 69x more likely to die than someone under the age of 40.
Pre-existing conditions (especially cardiovascular diseases and diabetes) have a similar impact and have likely played a role in the death of many of the relatively younger cases. And of course as you get older, there tends to be greater prevalence of pre-existing conditions — the two are related.
These exponential leaps in mortality rates by age (and existence of pre-existing conditions) are very much in line with recorded death rates from general pneumonia and seasonal flu, which makes complete sense because pneumonia — an infection of the lungs that causes inflammation of the lung — is what is causing the vast majority of COVID-19 fatalities.
Even at this early stage where there are still a lot of unknowns, I would highly recommend that older people or those with pre-existing conditions stay extra vigilant and heed recommendations from WHO and other authorities.
(3) Case Fatality Rate and importance of context
When confronted with something new like COVID-19, it is natural for many people to look to past epidemics as a basis for comparison. The most common ones that COVID-19 has been compared with are — by rough order of severity / global impact:
Regular flu (seasonal)
SARS (2003)
MERS (2015)
Swine Flu Pandemic (2009)
With these epidemics, on top of the R0 number mentioned earlier measuring contagiousness, the other number people latch onto is Case Fatality Rate (CFR), or the number of deaths per number infected (at least those that can be counted). A common chart I have seen is this:

On the one hand, you have seasonal flu which has an estimated CFR in the 0.10–0.14% range (Source: CDC, also here). Then you have MERS with a CFR of over 30% which is justifiably scary.
Currently the numbers based on confirmed COVID-19 cases in China are at 2.6% (as of February 17, 2020). 1,868 people have died out of 72,436 confirmed cases.
A natural instinct is to take this 2.6% number, multiply by an estimated number of infections, and figure out what the potential death totals may be. And based on the “highly contagious” nature of the disease — with credible experts estimating potential infection rates of 40-70% of global population — you arrive at some massive, panic-worthy numbers, fast.
But that is why context is so important. Once we start talking about total infections, 2.6% is likely the upper bound, and possibly too high by one or even two orders of magnitude. To understand why, we need to understand what the confirmed number actually represents.
The China CDC report provides an in-depth description of the process by which infections are confirmed. Originally, cases were only confirmed if a nucleic acid test on a throat swab sample came up positive. However, as the report describes, the procedure is “slow, labor intensive, and requires specialized equipment and skilled technicians”.
Given this was a new viral strain, and especially at the early stages of the crisis, there was limited capacity in how many lab tests could be done properly (and safely) every day.
Meanwhile, in Wuhan, the epicenter of the epidemic, local hospital and medical resources were hit hard by the sudden surge in cases. Not only were there limits on testing capacity, healthcare workers on the frontlines were contracting the virus (and likely passing it on to patients and each other): the China CDC report confirmed that 1,716 health workers were lab-confirmed with COVID-19, and 87% of these were in Wuhan or Hubei Province.
In other words, there was tremendous strain on local medical resources in Wuhan to not only diagnose and test patients, but to quarantine and care for sick patients as well. There are plenty of verified anecdotes that confirm that sick patients had to be turned away due to lack of capacity, including a prominent director and some of his immediate family members that were forced to self-quarantine.
This means that the cases that were confirmed and accepted into the overloaded local medical system were adversely selected for the most serious cases. And with the system under so much stress, there weren’t enough resources (both people and equipment) to care for those in the most critical condition — which invariably led to even higher mortality rates.
Update (2/18): Mike Ryan, Executive Director at the World Health Organization re-iterated these points at WHO’s most recent press conference (emphasis mine):
“… Remember at the beginning of the outbreak, what people were finding were the severe cases, so you have a huge bias at the beginning of the outbreak because what you find are the really sick people coming forward. And now we are going out looking for the less sick people …
… so you can have a … false sense of mortality at the beginning and we saw that … in the pandemic of H1N1 … we saw fatality rates of 10 and 20% in the beginning because only the severe cases were presenting and a few weeks later the pattern was entirely different.”
“There’s also the fact that the case fatality is different inside Hubei and Wuhan to the other provinces. And that may also reflect the fact that the pressure on the system in Wuhan and Hubei has been so severe and the lessons that have been learned … are being applied elsewhere and people are getting into earlier critical care.
One of the issues has been predicting patients who have the co-morbidities and underlying conditions and ensuring they are transitioned into the critical care or severe care pathway early and that we’re not blocking up the system with the mild cases. And I think the system in China … has gotten much better at prioritizing those more likely to be severely ill into the system.
It’s also very difficult in critical care to ventilate so many patients and do ECMO[23] with so many patients. It takes quite a lot of technical skill. It’s not just the machinery, it’s the technicans who use that. And again, bringing them up to speed, bringing in the emergency medical teams … remember 127 emergency medical teams, nearly 10,000 specialist medical workers were sent into Hubei from outside. Pre-trained, pre-certified medical teams who were used to mass casualty management. They would have helped to reduce case fatality.
So what we are seeing is a mixture of the fatality reducing probably because of better and better interventions over time but also because we’re finding more mild cases.”
So 2.6% is not a number that you can apply to the broad infected pool. A better way to think about it is as the mortality rate for an adversely selected pool of cases that is on balance significantly older and sicker than the general population.
Indeed, this adverse selection effect was demonstrated during the recent Swine Flu epidemic. As epidemiologists collected case information on the ground in the middle of the crisis, initial CFRs were calculated in the ~10% range. However, once researchers had time to properly estimate infection rates in the population (e.g. by looking for the presence of specific antibodies in blood), they realized that vast swathes of the population had gotten infected but had not exhibited serious enough symptoms to be counted — and the effective mortality rate plunged two orders-of-magnitude lower to ~0.1%.
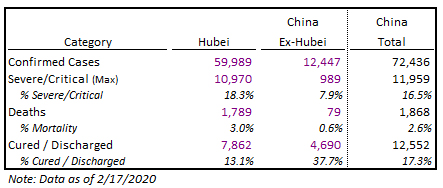
(4) The situation in Wuhan is very bad. But it may also (hopefully) be unique.
We can see just how different Hubei’s predicament looks from the rest of China, which had the benefit of greater awareness, the implementation of quarantines to slow the spread of infection, and less strain on local medical resources to identify and care for new confirmed cases. The differences in outcomes are about as clear as can be:
As we can see here, the mortality rate is significantly lower outside of Hubei, at 0.6%. The ratio of patients that have been cured and discharged to those who have died is almost 60:1.
Among patients that have yet to be discharged, the China CDC report encouragingly reported that “no deaths have occurred among those with mild or even severe symptoms”. Singapore’s Ministry of Health also independently reports that patients that are still hospitalized are “in stable or improving” condition and highly likely to survive.
Furthermore, the demographic information from cases outside of China (e.g. Singapore and Hong Kong) also show ratios that are more inline with China ex-Hubei than Hubei itself.
Indeed, the key lesson here may be that controlling this thing before it can get to such a critical mass that it overwhelms the local medical system and resources is extremely important.
And hopefully there is some light at the end of tunnel for Wuhan as it appears that officials are making progress working through some of the city’s capacity issues:
Conclusion
As I stated at the very beginning, there are still many unknowns out there. That is why there is no simple answer to the question of how dangerous this thing really is. Among others:
There is no vaccine against COVID-19 (one that can be deployed safely at scale)
We are still unsure about how contagious this is in people that are infected but asymptomatic
We do not know how many people are infected, because (very likely) many people are infected and not yet identified for a variety of reasons
We do not know exactly why infection and/or mortality rates for young people are so much lower
We do not know how countries with less-developed healthcare systems will be able to cope with potential outbreaks
SARS-CoV-2 will continue to mutate and evolve (although scientists aren’t that worried about this)
It’s hard to predict the second-order effects (e.g. policy under/over-reaction, economic disruption, etc.)
To make matters worse, with so much uncertainty on a topic that is highly technical and specialized — amplified by modern social media platforms which tend to reward simple and extreme vs. complex and nuanced — there is also a significant amount of misinformation out there. As discussed on a recent NPR podcast with Carl Bergstrom, professor at the University of Washington that studies the spread of scientific disinformation:
FADEL: What are the myths that are out there? Let's start there.
BERGSTROM: Well, there's a wide range of different stories that are out there. They range from misinformation about - simply about the rate at which the disease is spreading, misinformation about how many people it's killing. And then you get some really wild stuff out there like stories that it might have been a bio-weapon - it is not - sort of anything that could capture the imagination, get people scared, get people to spread them further.
FADEL: So what's behind all this disinformation, this misinformation? What's behind it?
BERGSTROM: This is a really fascinating case because there are a whole bunch of different sources of misinformation, and they have a whole bunch of different motives. Disingenuous actors - they want to spread misinformation to make China look as bad as possible and decrease trust of people within China for their own government and decrease trust from people outside of China for the Chinese government. They could potentially lead to various kinds of disruptions of, you know, normal international relations or normal international commerce and so forth.
FADEL: Right.
BERGSTROM: Then you get people that are simply spreading misinformation for profit, using this to sell, you know, snake oil treatments of various kinds. And then finally, there are a lot of well-meaning people that are scared and are not able to get good information and are sharing that because they're trying to take care of their friends and family, which is a very natural human emotion, of course.
FADEL: Why does this misinformation spread so quickly?
BERGSTROM: One of the things that's making the misinformation spread so quickly in this particular case is that there's a information vacuum. There's a ton of uncertainty surrounding what's actually going on with this virus. People are looking for answers that provide certainty. Most experts are unwilling to give answers like that because we simply don't know. I can give you a very broad range of how infectious the disease might be, how many people it might reach, how likely it is to kill you. But I can't give you a sharp number.
What people really want to hear are these sharp numbers, and if someone makes them up and states them in ways that seem authoritative, those are the kinds of pieces of misinformation that are likely to go spreading rapidly across social media.
All of this disinformation and noise leads to an entire spectrum of human emotional response from denial and anger to fear and outright panic. But excessive over-optimism or fear can both lead to sub-optimal outcomes. Over-optimism can lead to under-estimating or ignoring the potential risks. Panic can lead to “medicine” that harms the patient more than the disease itself.
And sadly, fear and anger have given way to xenophobia and racism, bringing out some of the worst of human nature.
At this point, the most important thing for us as a global society is to problem-solve together to clear as many of these unknowns as possible, as fast as possible. The public release of this comprehensive dataset and associated analysis is one big step to this end goal. But there is a lot more work to be done until we defeat this thing, not to mention codifying the lessons learnt so that we are better prepared to deal with the next one.
This was originally published on Quora on February 17th, 2020.